Radiation Therapy
Home » Braving Cancer Together » Prostate Cancer » Radiation Therapy

Radiation therapy delivered to the prostate is a form of curative treatment for prostate cancer. Radiation can be performed in several different modalities.

Brachytherapy
Brachytherapy involves the placement of seeds or very small metallic radiation sources into the prostate. The seeds stay in permanently, however the radiation goes away after a period of time. Good candidates for brachytherapy include men with low Gleason scores and a limited amount of cancer. Brachytherapy usually has less of an impact on sexual function than other forms of radiation. However, the recurrence rates are higher.
During the procedure, needles will be inserted into the skin between the rectum and the scrotum under ultrasound guidance to place the seeds. Patients will typically be under general anesthesia during the procedure. The planning of how much radiation is delivered is planned with the help of a physicist and x-rays are taken after placement to ensure proper placement.
Permanent brachytherapy usually requires an overnight hospital stay. After the procedure, patients may experience swelling and pain in the treatment area that may be addressed with over-the-counter pain medication and ice packs.
Risks of brachytherapy include an increase in bothersome urination, such as slow and incomplete emptying and more frequent nighttime urination. Other possible effects include urethral narrowing, rectal bleeding, blood in the urine, diarrhea, erectile dysfunction.
Another form of brachytherapy is known as high dose brachytherapy. During this operating room procedure, the temporary seeds are placed into the prostate and allowed to stay for a short period of time and then removed after delivering the radiation to the prostate. This type of treatment has a more limited experience without longer term outcomes.
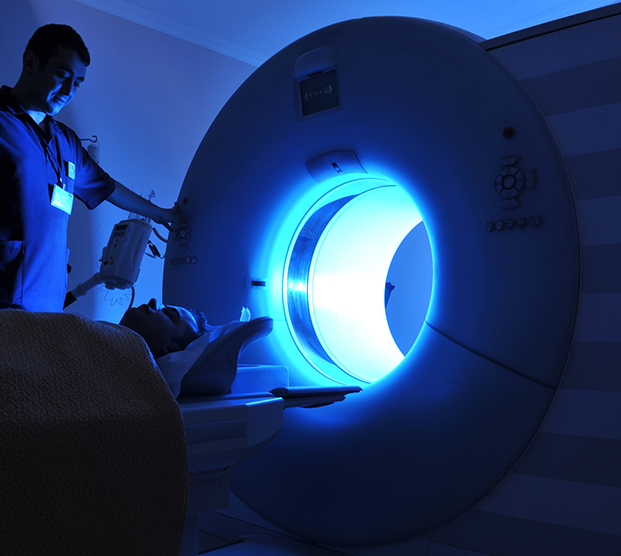

External Beam Radiation
External beam radiation therapy (EBRT) uses beams of radiation that are targeted at the cancerous organ. The techniques used during treatment allow extreme precision on the target while being able to minimize surrounding tissue damage. External beam radiation is typically in the form of electrons, however more recently proton therapy has been used. This has advantages in certain types of cancers but there have been no clear advantages seen for prostate cancer. Side effects include changes to urinary function and sexual difficulties.
Candidates for radiation therapy are typically comprised of older men with confined disease. Chances for cure are very high however for higher risk cases, hormonal therapy boosts the chances for cure and are thus used together.
The treatment course is usually five to eight weeks, with radiation administered five days a week during short and painless sessions. Typically, putting the body in the right position takes longer than administering the radiation itself. Patients are usually able to pursue their normal lifestyles during treatment.
Risks of external beam radiation therapy include urethral narrowing, erectile dysfunction, radiation cystitis and proctitis that can cause blood in the urine or stool with symptoms of irritation, urinary leakage and in the longer term cancer formation in the bladder or rectum.
Calypso/Fiducial Seed Placement
Before external beam radiation treatment begins, the Calypso Localization System or Cybermark Fiducial System may be implanted to consistently locate the prostate each day of treatment. The physician places three transponder “seeds” into the prostate to help identify the exact location of the gland. They are harmless and will remain in the prostate permanently.
SpaceOAR
Another procedure that can be done before radiation therapy is the placement of SpaceOAR an absorbable hydrogel that temporarily increases the space between the prostate and the rectum to help reduce the amount of radiation delivered to the rectum during treatment of the prostate. The gel is primarily made of water as well as biodegradable material that will be naturally absorbed by the patient’s body over time.
Reducing radiation dosing to the rectum may reduce tissue damage, decreasing the risk of complications and improving the quality of life for patients.
SpaceOAR is injected through a small needle using ultrasound imaging. The procedure may be done under local, regional, or general anesthesia.
